CIDP Awareness Month
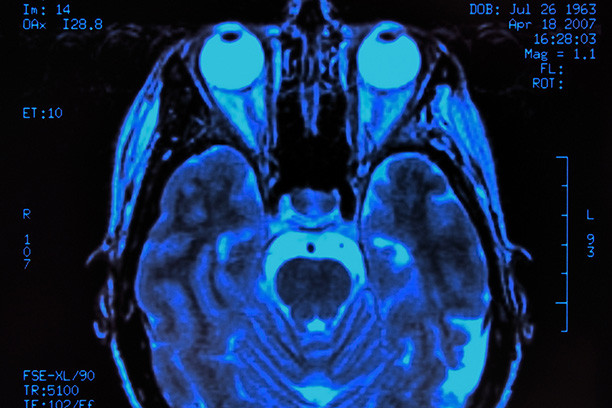
Vision Loss as a Presenting Feature of Chronic Inflammatory Demyelinating Polyneuropathy: A Case Series
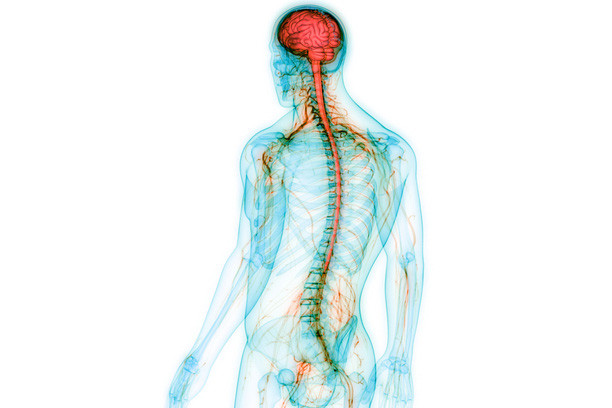
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired, immune-mediated, and clinically heterogeneous demyelinating disease affecting the nerve roots and peripheral nerves. We report a series of 4 patients who presented with early and progressive vision loss in the context of new-onset CIDP: 3 due to papilledema and 1 due to optic neuropathy without papilledema.
March 2023
Read moreRelated Articles
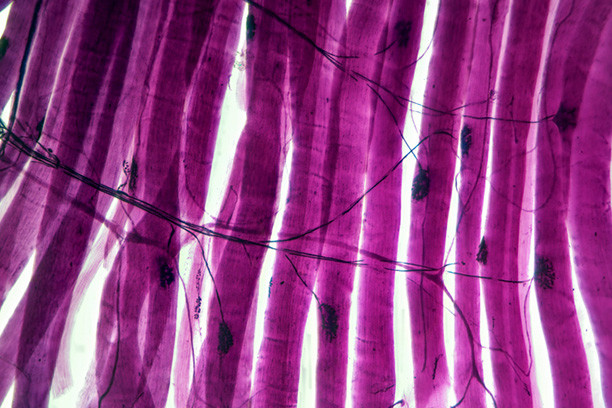
Nerve ultrasound for the diagnosis and follow-up of peripheral neuropathies
Cross-sectional area, echogenicity, morphology of the individual nerve fascicles, thickness of the epineurium, vascularization and mobility of the nerve are the main parameters evaluated with nerve ultrasound in polyneuropathies. Patients with typical chronic inflammatory demyelinating polyneuropathy show multifocal nerve enlargements easily visible on the upper extremities and the brachial plexus, whereas its variants show focal nerve enlargements
October 2023
Read moreFocused Neuromuscular Ultrasound Approach for the Diagnosis of Chronic Inflammatory Demyelinating Polyneuropathy
Previous ultrasonographic studies of individuals with chronic inflammatory demyelinating polyneuropathy (CIDP) have shown nerve enlargement at several sites. This prospective study compares only the bilateral median and ulnar nerves of individuals with CIDP with reference values to determine the clinical usefulness of this focused approach as a diagnostic tool.
May 2023
Read moreA Retrospective Study of Ultrasound Accuracy for the Diagnosis of Chronic Inflammatory Demyelinating Polyneuropathy
Ultrasound is emerging as a useful tool for the evaluation of immune-mediated neuropathies because it can provide high-resolution anatomic information to complement electrodiagnostic data. Nerve enlargements are commonly found in chronic inflammatory demyelinating polyneuropathy (CIDP), and their presence likely useful in diagnosis, particularly if multifocal.
May 2022
Read moreTendon-Sparing Extraocular Muscle Enlargement Associated With Chronic Inflammatory Demyelinating Polyradiculoneuropathy
Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is an inflammatory, sensorimotor polyneuropathy. It has presented with a variety of orbital and neuro-ophthalmic manifestations, including cranial nerve hypertrophy and a single case of extraocular muscle enlargement. The authors present a second case of tendon-sparing, extraocular muscle enlargement, resulting in new-onset diplopia and strabismus in a teenager with CIDP.
March/April 2024
Read moreWhat Is in the Literature
What is in the Literature focuses on chronic inflammatory demyelinating polyradiculoneuropathy (CIDP), a neuropathy with challenges in diagnosis and treatment. A recent revision of diagnostic criteria (EFN/PNS criteria) has helped define clinical features of typical and atypical variants and what is not considered CIDP. Initiating pathologic factors is not known for typical CIDP or variants.
December 2022
Read moreAtypical chronic inflammatory demyelinating polyradiculoneuropathy: recent advances on classification, diagnosis, and pathogenesis
Although the validity of the 2021 EFNS/PNS diagnostic criteria for atypical CIDP is unknown, they will hopefully lead to greater uniformity in the selection of patients to be enrolled in future studies and to a greater diagnostic accuracy. New data are emerging on the possible pathological mechanisms of individual variants and this could result in the discovery of specific diagnostic biomarkers and new therapies.
October 2021
Read moreNew-onset chronic inflammatory demyelinating polyradiculoneuropathy after COVID-19 infection: a case report
SARS-CoV-2 infection, besides respiratory symptoms, as cardinal manifestation, may present with neurological involvement. Immune-mediated polyradiculoneuropathy is one of the important neurological complications manifested by COVID-19 mainly includes Guillain–Barré syndrome (GBS), treatment-related fluctuation of GBS, and chronic inflammatory demyelinating polyradiculoneuropathy (CIDP).
October 2023
Read more